The Special Access Scheme (SAS) allows practitioners to import/gain access to therapeutic goods currently not registered on the Australian Register of Therapeutic Goods (ARTG) for a single patient on a case by case basis. Fosfomycin (one such SAS drug) is a broad spectrum antibiotic belonging to the phosphonic acid derivative drug class (other examples in this drug class include foscarnet and adefovir). Developed by Merck & Co. and Compañía Española de Penicilina y Antibióticos (CEPA) in 1969, fosfomycin is a bactericidal drug that disrupts cell wall synthesis by inhibiting phosphoenolpyruvate synthetase and thus disrupting peptidoglycan production. It has two oral forms (fosfomycin tromethamine and fosfomycin calcium) and one IV form (fosfomycin disodium).
In the USA, the FDA approved fosfomycin only for the treatment of patients with uncomplicated cystitis in 1996 but it has a history of use in European countries for a variety of indications including meningitis and initial empirical therapy for sepsis or soft tissue infections.

Figure 1. Fosfomycin dosing recommendations (Up-To-Date 2017)
A recent example case was a 71 year old woman who presented with a history of falls, fevers and a non-productive cough. She denied any urinary symptoms/abdominal pain/nausea or vomiting/coryzal symptoms/myalgias/arthralgias. Her history included hypothyroidism, parkinsonism, recurrent UTI, bipolar disorder, schizophrenia and cervical cancer.
Blood and urine cultures were taken and she was started on IV gentamicin and ampicillin. A multi-resistant Enterobacter cloacae was cultured (urine and blood) and a diagnosis of urosepsis was made. In the light of AST results directed therapy with meropenem 500 mg bd (eGFR 19) was prescribed.
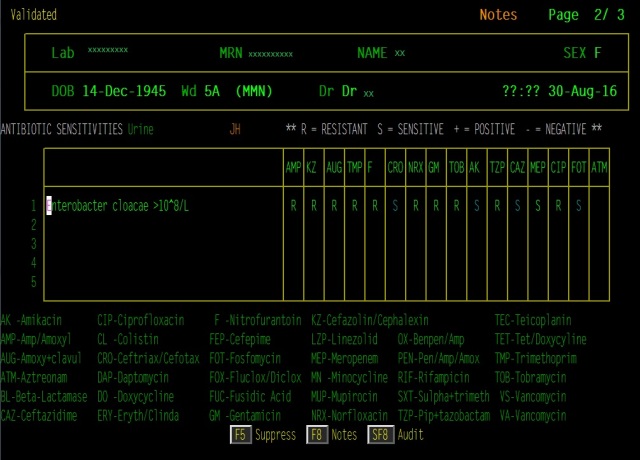
Figure 2. Susceptibilities of urine culture isolate
She was given fosfomycin 3g PO 72 hourly. She received two doses, clinically improved and was discharged a few days later to be followed up with a urologist as an outpatient.
Fosfomycin, like all other broad spectrum antibiotics, has the potential to lead to bacterial or fungal superinfection, including C. difficile-associated diarrhoea and pseudomembranous colitis. While resistance to fosfomycin has been shown to be low, ESBL producing strains of pathogens have been identified in bacteria with particular genes including Escherichia coli (fosA, fosC), Enterobacter cloacae (fosA), Klebsiella pneumoniae (fosA), and Staphylococcus spp. (fosB). These fosfomycin resistant genes confer substantially higher MICs and may transfer through multiple genetic mechanisms – two of them located on the chromosome and the third of plasmid origin.
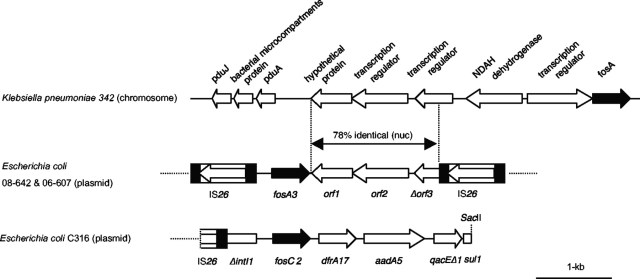
Figure 3. Example of fosfomycin resistance transfer E. coli to K. pneumoniae via plasmid (Wachino 2010)
Fosfomycin certainly has current clinical value – in particular in multi-drug resistant organism (MDRO) cases. It has shown antimicrobial activity against biofilms, particularly in combination with fluoroquinolones or aminoglycosides and has shown excellent bactericidal activity against gram-positive cocci and many gram-negative bacteria. No adjustments are needed in case of renal/hepatic impairment, it has minimal drug-drug interactions and minimal contraindications.
Fosfomycin is a restricted antimicrobial and its use should be discussed with the ID or Clinical Microbiologist services (at JHH and CMN it needs registering on GuidanceMS).
References:
-
Alrowais, H., McElheny, C.L., Spychala, C.N., Sastry, S., Guo, Q. and Butt, A.A., 2015. Fosfomycin resistance in Escherichia coli, Pennsylvania, USA. Emerging infectious diseases, 21(11), pp.2045-2047.
- Michalopoulos, A.S., Livaditis, I.G. and Gougoutas, V., 2011. The revival of fosfomycin. International journal of infectious diseases, 15(11), pp.e732-e739.
-
Wachino, J.I., Yamane, K., Suzuki, S., Kimura, K. and Arakawa, Y., 2010. Prevalence of fosfomycin resistance among CTX-M-producing Escherichia coli clinical isolates in Japan and identification of novel plasmid-mediated fosfomycin-modifying enzymes. Antimicrobial agents and chemotherapy, 54(7), pp.3061-3064.
-
Xu, Xiaogang, et al. “The fosfomycin resistance gene fosB3 is located on a transferable, extrachromosomal circular intermediate in clinical Enterococcus faecium isolates.” PloS one 8.10 (2013): e78106.
Hi,
Thanks for the lovely blog. It’s a useful antibiotic to be used sparingly. I have used it as well for sepsis in combination with chloramphenicol for ITU/solid organ transplant/immunocompromised patients and its worth keeping up your sleeve if first line doesn’t work.
Regards
Ling
LikeLike
Hi Ling,
I agree, useful but to be used sparingly. Interesting that you use it in solid organ transplant, if you ever felt like writing a post about your experience with fosfomycin or any other antimicrobials in your field we would be glad to hear from you. Either way, thanks for the comment!
Kind Regards,
Sim
LikeLike
[…] to administer intravenous antibiotics or to get permission to use an oral antibiotic (fosfomycin) that is not yet licensed in Australia. Both are expensive and inconvenient […]
LikeLiked by 1 person
[…] to administer intravenous antibiotics or to get permission to use an oral antibiotic (fosfomycin) that is not yet licensed in Australia. Both are expensive and inconvenient […]
LikeLike
[…] Fosfomycin is available in Australia as an oral formulation for resistant UTIs. Intravenous fosfomycin in going to the FDA for UTI – note that susceptibility testing is not properly validated and gives conflicting results – labs need to use a complex method called agar dilution to reliably test for resistance. See also this posting. […]
LikeLike