Tag Archives: Staphylococcus aureus
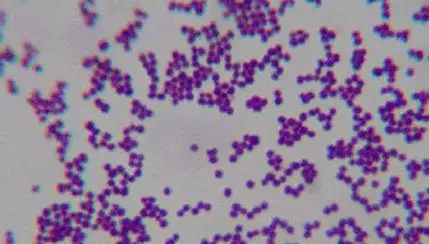
Preoperative nasal screening for Staph. aureus carriage and load reduction (HNE LHD)
Indications for preoperative screening for Staphylococcus aureus (MSSA or MRSA) nasal carriage and preoperative staphylococcal load reduction (HNE LHD): Open cardiac and valve procedures Shoulder, hip or knee joint total arthroplasties: primary or revision procedures Aortic work (stent and open) and all lower limb open surgery for vascular reconstructions (bypass, endarterectomy). Iliac stents (as they […]
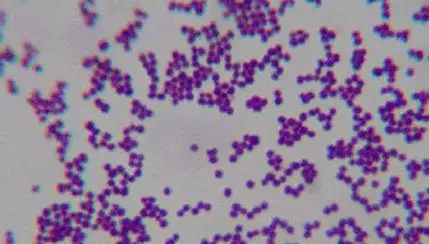
Relapse of Staphylococcus aureus bloodstream infection – patient information sheet
Staphylococcus aureus bloodstream infection (septicaemia) information card [Patient Label ] [ [ You were recently diagnosed with a blood infection caused by a bacterium called Staphylococcus aureus (“Golden Staph”). This infection has been treated with intravenous antibiotics. Whilst this usually cures the infection, there is a possibility that your infection could return within 3 months […]
Q2 Understanding antibiotic resistance and Staphylococcus aureus
Q2 in our JMO pre-test asked: “What is the main mechanism by which the bacterium Staphylococcus aureus becomes resistant to penicillin?” We gave alternatives enumerating basic mechanisms that micro-organisms use (often in combination) to become resistant to an antimicrobial agent (graphic below). Production of penicillinase (i.e. inactivation by a type of beta-lactamase) was the correct answer– more […]

Flucloxacillin is highly effective against Streptococcus pyogenes (group A strep) and related species
A common myth – “Flucloxacillin and penicillin in combination are required to treat cellulitis” NOT TRUE: monotherapy is adequate.
Essential clinical care of Staphylococcus aureus bloodstream infection (SAB)
Updated 8/5/20. A. Healthcare-associated events (2018, HNE LHD ) 60 healthcare-associated SAB cases occurred with 7% due to methicillin-resistant Staphylococcus aureus (MRSA) and age-adjusted 30 day mortality of 9%. SAB relapse within 15-90 days occurred in 2.1% of adult events 7% of paediatric events. Principle sites common: ● Vascular access device (e.g. intravenous cannula, central […]