Category Myths & Misconceptions
Let’s stop using antibiotics for uncomplicated diverticulitis
Guest posting : Dr Daniel Isacson, local GP (ex Swedish researcher) The evidence is out and there is no proven benefit in recovery or complication rates in treating these patients with or without antibiotics, but still many GPs and surgeons prefer to use antibiotics. How do we get the word across?

Recurrent urinary tract infection in women – are antibiotics the answer?
What is the evidence? This interesting paper from 2010 discusses the natural history of UTI in women and distinguishes two conditions – the ‘urethral’ (or ‘dysuria/frequency’) syndrome’ (US) which affects a proportion of women with recurrent symptoms and many courses of treatment. It is known that US is a self-limited condition in a majority of patients. Some women are said to […]

Is penicillin enough for aspiration pneumonia?
There has been quite a tradition for including Gram negative anaerobic cover for patients suspected to have aspiration pneumonia. There are virtually no randomised trials that directly address the issue with nearly all such trials including agents that have Gram negative anaerobic cover across all treatment arms. One exception was a small trial from 1997 in a paediatric […]

Is ceftriaxone a good anxiolytic for prescribers faced with diagnostic uncertainty ?
The adult presented with 1 week of non-productive cough (yes, a good history was taken), and had no signs of sepsis other than fever. CRP moderately raised, CXR normal. The clinician documented a vague differential diagnosis and started ceftriaxone.
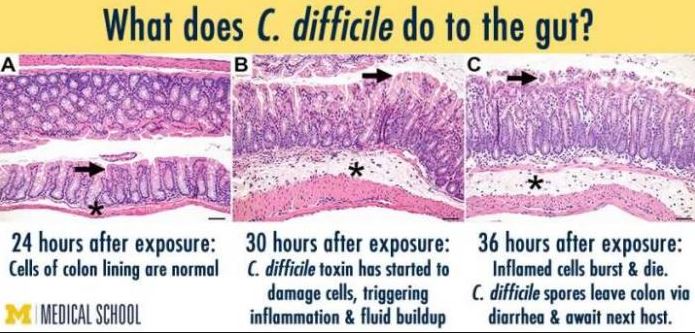
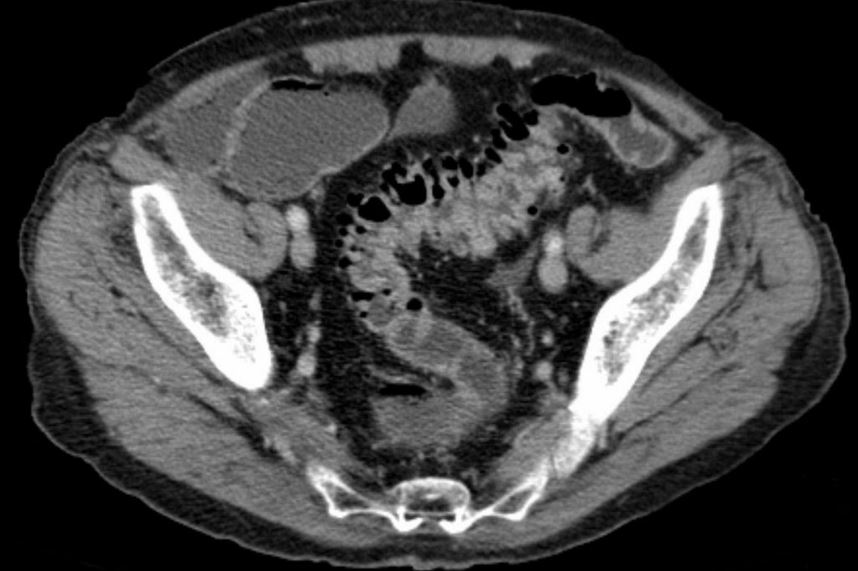
Clostridium difficile – misconceptions about testing
Confine testing to symptomatic patients. Testing of patients with formed stools may generate false positives due to asymptomatic carriage of toxigenic strains. An unfortunate side effect of multiplex PCR stool assays, are that tests that are inappropriate to the clinical circumstance may be performed, generating false positives. Also test at-risk (i.e. antibiotic or ppi-exposed) symptomatic […]

Bronchiectasis and goals of antibiotic treatment – thinking it through
The setting – patients with bronchiectasis (including those with cystic fibrosis) have impaired respiratory secretion clearance and a vastly different lower respiratory flora (microbiome) than patients with normal lungs. They are frequently colonised with conventional respiratory species such as Haemophilus influenzae and Moraxella catarrhalis, Staphylococcus aureus, a diverse range of Gram negative bacteria and even fungi. Colonisation/infection with non-tuberculous […]
Tazocin misconceptions: misuse in community-acquired pneumonia – spectrum too broad
Piperacillin+tazobactam (Tazocin) is an important broad spectrum antibiotic that is still active in most Australian settings against a wide range of Gram negatives (including Pseudomonas) , Gram positives (excluding MRSA and VRE) and nearly all anaerobic bacteria. It comes into great demand for management of a range of healthcare-associated infections, especially in ICU. Its use […]
Diagnostic error is a major factor leading to inappropriate antimicrobial use- recent landmark paper
Diagnostic accuracy is a factor neglected by most antimicrobial stewardship programs and should perhaps be subject to regular audit and feedback. It is heavily dependent upon the context of the clinical contact – for example, time-pressured, after hours hospital ward patient encounters are prone to quick judgements and sloppy diagnoses. For a persuasive discussion of […]
Do you really need to finish that antibiotic course?
Professor Lyn Gilbert started a discussion going with her recent MJA piece. Health and Wellbeing (ABC) took up the discussion with a further piece teasing out some of these issues- Antibiotics – when is enough enough? Full text below. The community discussion that followed on the ABC News Facebook page was very interesting and diverse! […]

Flucloxacillin is highly effective against Streptococcus pyogenes (group A strep) and related species
A common myth – “Flucloxacillin and penicillin in combination are required to treat cellulitis” NOT TRUE: monotherapy is adequate.